The TASC II (Transatlantic Inter-Society Consensus for the Management of Peripheral Arterial Disease) consensus document addresses aspects of revascularization in PAOD.
The TASC II criteria recommend therapeutic treatment options depending on the length of the local occlusion/stenosis. The length of the stenosis and its regional location determine the treatment: endovascular or open vascular surgery.
TASC II classification of femoropopliteal lesions
Type | Morphology | Procedure |
A | Unilateral or bilateral stenosis of CIA; unilateral or bilateral single short (<3 cm) stenosis of EIA | Endovascular |
B | Short (≤3 cm) stenosis of infrarenal aorta; unilateral CIA occlusion; single or multiple stenosis totalling 3–10 cm involving the EIA, not extending into the CFA; unilateral EIA occlusion not involving the origins of IIA or CFA | Endovascular |
C | Bilateral CIA occlusion; bilateral stenoses 3–10 cm long, not extending into CFA; unilateral EIA stenosis extending into the CFA; unilateral EIA occlusion involving the origins of IIA and/or CFA; heavily calcified unilateral EIA occlusion with/without involvement of origins of IIA and/or CFA | Open revascularization |
D | Infrarenal aortoiliac occlusion; diffuse disease involving the aorta and both iliac arteries requiring treatment; diffuse multiple stenoses involving the unilateral CIA, EIA, and CFA; unilateral occlusions of both CIA and EIA; bilateral occlusions of EIA; iliac stenoses in patients with AAA requiring treatment and not amenable to endograft placement; or other lesions requiring open aortic or iliac surgery | Open revascularization |
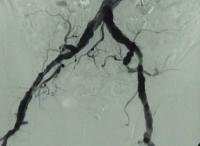
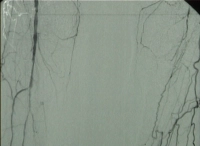
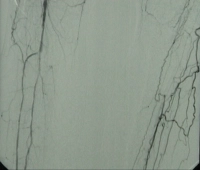
Video example: TASC D → open repair
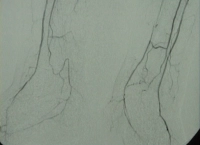
Right leg PAOD Fontaine grade IV, left leg grade III with:
- High-grade arteriosclerosis of the terminal aorta and both iliac arteries
- Extended occlusion of both superficial femoral arteries
- Partial occlusion of the infrapopliteal arteries in bith legs
Preoprative DSA: