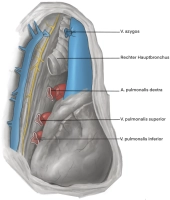
In a pneumonectomy, the supplying structures in the hilum are resected. Here, the central pulmonary artery, the superior and inferior pulmonary veins, and the right main bronchus must be isolated, preparated, and transected.
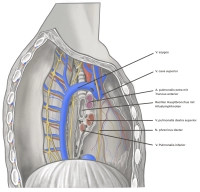
During the preparation of the right lung hilum from the ventral side, the following key structures become visible after transecting the mediastinal pleura:
- The right pulmonary root is located dorsolateral to the superior vena cava, and the phrenic nerve runs ventrally between the pericardium and mediastinal pleura.
- The azygos vein drains into the superior vena cava above the right main bronchus.
- The pulmonary artery is located cranially and dorsally to the superior pulmonary vein.
- At the lower end of the superior pulmonary vein, the two middle lobe veins or their common trunk drain.
- The inferior pulmonary vein is usually not directly visible from the ventral side.