Primary Gastric Carcinoma
In a curative therapeutic approach and local resectability, there is generally an indication for surgery, provided there are no significant risk factors (e.g., pre-existing conditions or the general condition of the patient; see also contraindications).
For locally advanced tumors of stages II and III (cT1/cT2N+ and cT3/resectable cT4Nx), pre- or perioperative chemotherapy should be performed.
To achieve tumor-free resection margins (R0), a proximal safety margin of 5 cm (for the intestinal type according to Lauren) or 8 cm (for the diffuse type according to Lauren) is generally required, except for mucosal carcinomas (T1a N0 M0). The extent of resection (total versus subtotal gastrectomy) is determined by the tumor location and spread, as well as the histological type, which requires an appropriate safety margin.
Early Gastric Carcinoma
An early gastric carcinoma is defined as a tumor that, regardless of lymph node status, surface area, and distant metastasis, is confined to the mucosa and submucosa of the stomach wall. The muscularis propria of the stomach is tumor-free by definition.
In early carcinomas, the frequency of lymph node metastasis varies. Tumors that have already infiltrated the submucosa are not eligible for endoscopic therapy, as there is a 4-20% probability of lymph node metastasis.
About 5% of patients show an early gastric carcinoma of the mucosal type (pT1m), where curative therapy through endoscopic resection is possible, as the probability of lymph node metastasis is extremely low. Affected patients have an excellent prognosis with a five-year survival rate of over 90%.
Indications for Endoscopic Resection
Superficial gastric carcinomas confined to the mucosa (about 5% of patients) can be treated with endoscopic resection considering the following criteria:
- Lesions < 2 cm in size for elevated types
- Lesions up to 1 cm in size for flat types
- Histological differentiation grade: well or moderately (G1/G2)
- No macroscopic ulceration
- Invasion confined to the mucosa
Special Situations:
Gastric Stump Carcinoma (Recurrent Tumors after Subtotal Gastrectomy):
Completion gastrectomy resulting in total gastrectomy.
Oligometastasis:
As part of a multimodal approach, within studies and when technically feasible, all metastatic sites can be removed. Metastases discovered intraoperatively can, similar to the esophageal guideline, be resected if they are R0-resectable.
Peritoneal Metastases:
Requirements:
- PCI < 12
- Complete resection of all macroscopically visible tumor parts possible
Procedure:
- Neoadjuvant systemic therapy
- Oncological resection (gastrectomy/subtotal gastric resection) with D2 lymphadenectomy and tumor-free resection margins
- Complete resection of peritoneal metastases (cytoreductive surgery)
- Hyperthermic intraperitoneal chemotherapy
In a palliative therapeutic approach, gastrectomy may be indicated in rare cases (e.g., in bleeding, perforation, stenosis).
Lymphadenectomy
The lymph node dissection of compartments I and II is referred to as D2-LAD and represents the standard lymphadenectomy for gastric carcinoma. It is considered the gold standard.
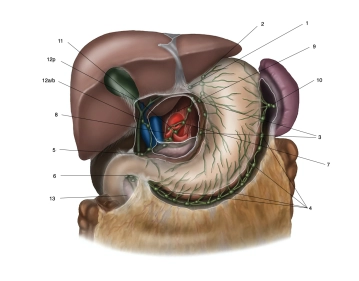
Based on the Japanese classification (numbering), the lymph nodes are grouped into several compartments. The D1 lymph nodes include stations 1 to 6, the D2 compartment additionally includes stations 7 to 11.
The lymph nodes of station 12 are resected in the context of oncological resection for distally located carcinomas on the lesser curvature side. Lymph nodes at the main bile duct (station 12b, considered M1) are often not resected to avoid injury/devitalization of the bile duct.
In the D3 compartment, groups 12 to 15 are located, which by definition are not regional lymph node stations of the stomach. As they are prognostically considered distant metastases, they are classified as M1 LYM if involved.
To achieve a classification of pN0, the UICC requires a minimum of 16 regional lymph nodes to be examined. The German S3 guideline specifies an intended lymph node count of ≥ 25.