The repair of inguinal hernia is the most common operation in visceral and general surgery. The lifetime risk for men is 27%, for women 3%.
The incidence increases with age, and patients with a positive family history are significantly more affected.
Risk factors include:
- COPD
- Nicotine abuse
- Reduced BMI
- Collagen diseases
Indirect inguinal hernias occur twice as often as direct ones. Femoral hernias account for only 5% of inguinal hernias. Right-sided hernias are more common than left-sided ones.
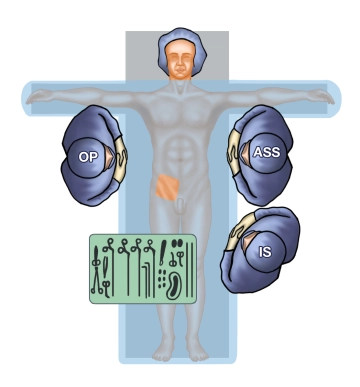
EHS Classification of Inguinal Hernias
Classification | Size | M = Medial | L = Lateral | F = Femoral | C = Combined |
I | < 1.5 cm |
|
|
|
|
II | ≥ 1.5 - 3 cm |
|
|
|
|
III | ≥ 3 cm |
|
|
|
|
Recurrence | R* 0-x |
|
|
|
|
There is no general recommendation for surgical therapy in the case of mildly symptomatic or asymptomatic, non-progressive inguinal hernia in men. Since most patients develop symptoms over time, it is recommended to discuss the indication for surgery and the timing with the patient, taking into account health status and social circumstances; "watchful waiting" may be an option.
The data on recurrent hernia is not as clear, so surgery is more likely to be recommended even for asymptomatic, non-progressive hernia.
In women, femoral hernias occur more frequently than in men. Since no diagnostic procedure can reliably distinguish between inguinal and femoral hernias and femoral hernias incarcerate significantly more often than inguinal hernias, the indication for surgical repair of hernias in women should be made promptly.
In general, a mesh-based surgical procedure is recommended for the treatment of inguinal hernia.
A non-mesh method should only be chosen if the patient refuses a mesh or if no mesh is available.
For primary unilateral inguinal hernia in men, a laparoendoscopic approach is preferred due to the lower incidence of postoperative pain. If the surgeon lacks sufficient experience or the necessary resources, the Lichtenstein operation is the alternative.
The Lichtenstein operation is recommended in the guidelines as the best open procedure currently available for the treatment of primary unilateral inguinal hernias in adults. After the Lichtenstein operation, recurrence rates are significantly lower than after suture techniques (Bassini and Shouldice) and comparable to those of laparoendoscopic procedures.
Approach to Primary Inguinal Hernia
| conservative | operative | open/anterior approach | laparoscopic/endoscopic |
|---|---|---|---|---|
unilateral hernia in men asymptomatic/non-progressive | + | + | + | + |
unilateral hernia in men symptomatic and/or | - | + | + | + |
bilateral hernia in men asymptomatic/non-progressive | + | + | - | + |
bilateral hernia in men symptomatic and/or | - | + | - | + |
hernia in women, unilateral/bilateral/asymptomatic/ | - | + | - | + |
In about 40% of recurrence operations after Lichtenstein surgery in women, a femoral hernia is found, suggesting that it was an overlooked femoral hernia during the primary operation. A possible explanation is that the transversalis fascia is not opened, and thus no exploration of the preperitoneal space occurs. Therefore, guidelines recommend posterior procedures with exploration of the femoral defect, namely the laparoendoscopic mesh procedures TEP and TAPP.
Plug and patch techniques and bilayer (double mesh) methods are not recommended due to the excessive use of foreign material and because the anterior and posterior anatomical layers are covered with mesh material. This makes any recurrence operations more difficult because no untouched layer remains.
Recurrent Inguinal Hernia
All guidelines recommend a laparoendoscopic approach for a recurrence after an anterior suture or mesh procedure. The advantage is the dissection in the previously unaffected anatomical layer. Conversely, for a recurrence after a posterior procedure, an anterior procedure (Lichtenstein) should be applied.
In principle, laparoendoscopic techniques are preferred over the Lichtenstein operation due to less postoperative and chronic pain. Nevertheless, there are hernia characteristics that make the Lichtenstein technique the first choice:
- Patients with increased perioperative risks
- severe comorbidities without the possibility of general anesthesia, especially in cardiopulmonary risk patients (ASA stage III/IV), here surgery in local or epidural anesthesia
- after previous operations in the small pelvis (radical prostatectomy, cystectomy, vascular interventions)
- scrotal hernias (EHS L3 and M3: defect > 3 cm)
- recurrence after laparoscopic/endoscopic procedure (TEP/TAPP)
- ipsilateral kidney transplanted patients
- patients with peritoneal dialysis
- patients with ascites
- anticoagulated patients
- upcoming pelvic radiation
- limited medical-surgical resources
Approach to Recurrent Inguinal Hernia
| conservative | operative | open/anterior approach | laparoscopic/endoscopic |
|---|---|---|---|---|
hernia asymptomatic/non-progressive after anterior approach | +? | + | - | + |
hernia asymptomatic/non-progressive after posterior approach | +? | + | + | (+) |
hernia symptomatic/progressive after anterior approach | - | + | - | + |
hernia symptomatic after posterior approach | - | + | + | (+) |
? = adequate expertise in laparoscopic hernia surgery required
In incarcerated inguinal hernias, which are distinguished from irreducible hernias by pronounced pain, acute onset, and signs of bowel obstruction, the diagnostic superiority of laparoscopy should be utilized. Its advantage is the possibility of repositioning the incarceration with assessment of organ perfusion afterward. In about 90% of cases, organ perfusion recovers after repositioning.
The repair of the inguinal hernia can be performed depending on the local infection situation either immediately or at a later time. In principle, a Lichtenstein repair is also possible if bowel resection is necessary.
The case presented in the teaching contribution shows the operation of a medial/direct hernia. To also address the repair of an indirect hernia, we will exemplarily discuss the approach to an indirect hernia sac through video sequences from another operation in step 7.