In terms of function, the stomach mixes and stores food and is an expansion of the alimentary tract between the esophagus and the duodenum. This muscular hollow viscus produces acidic gastric juice (mucus and HCl) and enzymes, which predigest some elements of the ingested food, and portions the chyme into the duodenum.
Usually, the stomach is located immediately inferior to the diaphragm in the left upper quadrant and epigastrium. Location, size and shape of the stomach vary from person to person and may differ substantially, depending on age, filling condition and body position. The moderately filled stomach has a mean length of 25- 30 cm and can hold 1.5 liters, in extreme cases up to 2,5 liters.
Within the abdominal cavity the stomach is held in position and stabilized by ligaments inserting at the liver and spleen Its convex aspect forms the major curvature (curvatura major gastrica) and its concave aspect the lesser curvature (curvatura minor gastrica). Its anterior wall is termed paries anterior gastrica and its posterior aspect paries posterior gastrica.
Since the stomach is an intraperitoneal viscus, it is covered by the gastric serosa (tunica serosa gastrica), and only the posterior aspect of the cardia is free of serosa. Stomach rotation shifts the embryonic mesogastrics from their former sagittal position to a frontal location. The lesser omentum originates at the lesser curvature and extends to the hepatic portal, while the greater omentum originates at the greater curvature and courses to the transverse colon, spleen and diaphragm.
The stomach displays the following portions:
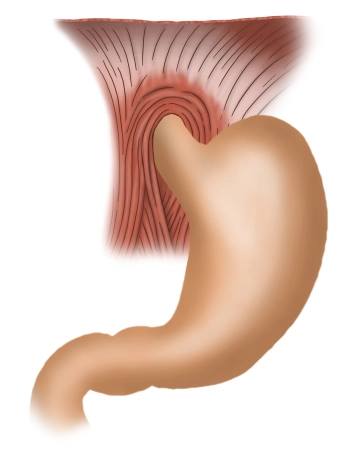
Entrance of stomach / Cardia / Ostium cardiacum:
The superior opening of the stomach, where the esophagus enters the stomach, is 1- 2 cm long. It is characterized by a marked transition from the mucosa of the esophagus to that of the stomach.
Gastric fundus / fundus gastricus:
Superior to the level of entrance of the esophagus the fundus arches cephalad, which then is called gastric fornix (fornix gastricus). Usually, the fundus is full of air which is swallowed automatically when ingesting food. In the erect position the fundus is the highest point of the stomach, and on abdominal films its trapped air is evident as the “gastric bubble”. A notch (incisura cardialis) clearly delimits the fundus from the entrance of the stomach.
Body of the stomach / Corpus gastricum
The main portion of the stomach is taken up by the gastric body. The deep mucosal folds (plicae gastricae) found here extend from the cardia to the pylorus and are also known as “magenstrasse”.
Pylorus / Pars pylorica:
This portion begins with the extended pyloric antrum, followed by the pyloric canal, and terminates at the actual pylorus. It is formed by the pyloric sphincter (m. sphincter pyloricus), a strong circular layer of muscle which closes off the inferior gastric orifice (ostium pyloricum). The pylorus closes off the gastric outlet and periodically lets some of the chyme pass into the adjacent duodenum.