- The gallbladder stores bile produced by the liver and releases it as needed. Additionally, it concentrates the bile by removing water and NaCl, reducing its volume to up to 10% of the original.
- Bile is released by the gallbladder in response to the presence of dietary fats, which require emulsification into digestible components.
- Stimuli for bile release include cholecystokinin and increased parasympathetic activity. These triggers cause gallbladder contraction, leading to bile flow through the cystic duct into the common bile duct and finally into the duodenum.
- In this manner, bile contributes to the digestion of high-fat foods.
-
Function of the Gallbladder and Bile
-
Macroscopic Anatomy of the Gallbladder
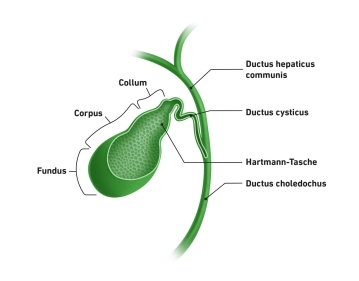
![510_AN_01.jpeg]()
- The gallbladder is an intraperitoneal organ located beneath the liver, adjacent to liver segment V, within the biliary fossa on the visceral surface of the liver.
- It measures approximately 10 cm in length and 4 cm in diameter, with a pear-shaped form.
- Its yellow-green, viscous bile gives the gallbladder a similar coloration.
- Capacity: Approximately 70 ml
- Anatomical structure: neck (collum), body (corpus), and fundus.
- Anatomical relations:
- Neck: Ventral to the superior duodenum.
- Body: In contact with the right colic flexure.
- Fundus: Projects below the liver’s inferior margin, to the right of the falciform ligament, at the level of the 9th rib.
- Closure Mechanism:
- The gallbladder neck and cystic duct contain a spiral mucosal fold, the Plica spiralis (Heister valve), regulating bile flow.
- The Hartmann’s pouch, is a bulging at the infundibulum near the cystic duct.
-
Biliary Anatomy
- The bile ducts originate intrahepatically from the right and left hepatic ducts (Ductus hepaticus dexter et sinister), which merge into the common hepatic duct.
- The cystic duct from the gallbladder joins this to form the common bile duct (Ductus choledochus), which empties into the duodenum at the major duodenal papilla (Vater’s papilla).
- The bile flows from the hepatic ducts and cystic duct into the gallbladder.
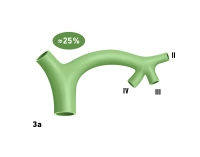
- The left hepatic duct (Ductus hepaticus sinister) is 3-5 cm long and is formed in the umbilical fissure by the convergence of ducts from segments II and III. Proximal to this junction, the bile duct from segment IV is usually incorporated.
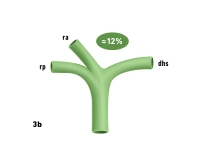
The right hepatic duct (Ductus hepaticus dexter) is shorter and occasionally absent, with anterior and posterior branches draining segments V-VIII directly into the common hepatic duct.
Anomalies:
- Variations in the cystic duct are rare but can have significant implications, especially regarding potential injury to the common bile duct. The cystic duct can vary in length, merge with the bile duct at different points, or share a common wall with it.
- Accessory bile ducts may connect the liver to the cystic duct, gallbladder, or right hepatic duct.
Clinical Tip: If the cystic duct is not clearly identifiable, the gallbladder can be opened, and the duct probed internally. Alternatively, ICG imaging or intraoperative cholangiography can clarify anatomy.
Clinical Tip: Injuries to the common bile duct (Ductus choledochus) often occur due to anatomical anomalies or disease-related changes. Excessive traction on the cystic duct risks injury to the common bile duct by inadvertently including its edge during ligation, potentially causing transection or stenosis.Left Hepatic Duct (Ductus hepaticus sinister)
- The most common (approximately 25%) and clinically significant variant involves a shared confluence of the segment IV bile duct with ducts from segments II/III (Fig. 3a).
- During left-lateral liver resections, living donor liver transplants, or liver splitting procedures, bile flow from segment IV can easily be compromised.
Right Hepatic Duct (Ductus hepaticus dexter)
- Occasionally, the right hepatic duct may be very short or absent. In such cases, the anterior and posterior pedicles of double segments V/VIII and VI/VII originate directly from the common hepatic duct (Fig. 3b), and the typical bifurcation of the hepatic ducts is absent.
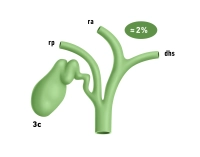
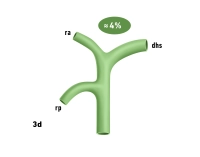
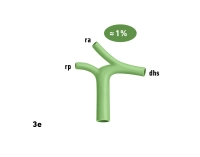
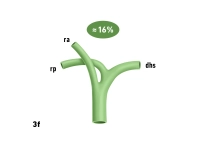
Figures 3b to 3g: rp = Right posterior bile duct, ra = Right anterior bile duct, dhs = Left hepatic duct.
Variations in Confluences
- Posterior bile duct draining directly into the cystic duct, common hepatic duct, or common bile duct (Fig. 3c-d).
- Anterior and, more frequently, posterior right bile ducts draining into the left hepatic duct (Fig. 3e-g).
- Clinical Relevance in Left Hepatectomy: Accidental transection of bile ducts due to such variations can lead to significant bile leakage and segmental cholestasis in the right liver lobe.
-
Microscopic Anatomy of the Gallbladder Wall
- Wall thickness: <4 mm when filled (preprandial), <8 mm when empty (postprandial).
- The wall forms folds and crypts (Rokitansky-Aschoff crypts), varying with the degree of distension.
Layers
- Tunica mucosa: Single-layered cylindrical epithelium, lamina propria
- Tunica muscularis: Obliquely arranged smooth muscle
- Tela subserosa: Connective tissue layer between muscularis and serosa
- Tunica serosa: Facing the peritoneal cavity
- Tunica adventitia: Facing the liver
Arterial supply:75% by a single cystic artery originating from the right hepatic artery (posterior
Activate now and continue learning straight away.
Most popular offer
webop - Savings Flex
Combine our learning modules flexibly and save up to 50%.
US$52.30/ yearly payment
robotics
Unlock all courses in this module.
US$104.60 / yearly payment