A hiatal hernia occurs due to a weakening of the diaphragm, where varying portions of the stomach, up to the entire stomach in severe cases, along with the spleen and intestinal parts, may shift into the thoracic cavity through a gap between the diaphragm's crura.
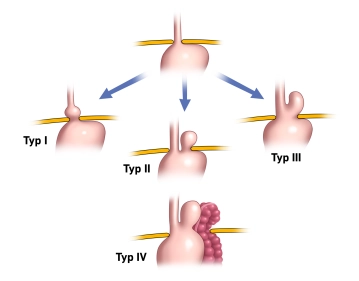
There are 4 types distinguished
Type I: Axial hernia, meaning the stomach entrance moves along the organ's axis through the hiatus upwards.
Type II: Paraesophageal hernia, meaning the stomach entrance remains below the diaphragm while other parts of the stomach move alongside the esophagus through the hiatus into the thoracic cavity.
Type III: Mixed form of Type I and II. There is both an axial shift of the esophagus and stomach towards the thoracic cavity and a displacement of stomach parts up to the entire stomach alongside the esophagus (thoracic stomach – "upside-down stomach").
Type IV: The most severe form, where additionally parts of the colon, the spleen with or without the pancreatic tail, are displaced into the thoracic cavity.
Axial sliding hernias account for up to 90% of cases and are initially described as a normal variant rather than a disease per se.
The indication for surgery depends on the symptomatology and hernia morphology.
While the goal of antireflux surgery is to strengthen the lower esophageal sphincter with a gastric wrap to prevent reflux, the goal for hiatal hernias of Types II-IV is to correct the incorrect position of the stomach and other organs displaced into the thoracic cavity.
An indication for surgery exists for:
- Axial hiatal hernia with therapy-resistant reflux disease
Note: An antireflux operation should only be performed if there is a long-term need for therapy (>1 year).
- Complicated GERD ("gastroesophageal reflux disease"): severe reflux esophagitis (Los Angeles Grade C and D), peptic stricture
The Los Angeles classification is the most commonly used grading system for reflux esophagitis. The Los Angeles classification is based on the endoscopic examination of the esophagus. It distinguishes 4 stages:
- Stage A: One or more mucosal lesions < 0.5 cm. The lesions do not extend beyond the tops of two mucosal folds.
- Stage B: At least one lesion > 0.5 cm. However, the lesions do not yet extend beyond the tops of two mucosal folds.
- Stage C: The lesions extend beyond the tops of several (>2) mucosal folds. However, they occupy less than 75% of the total circumference of the esophagus, i.e., there are no circular defects yet.
- Stage D: There are circular lesions that occupy more than 75% of the total circumference of the esophagus.
- Disease not completely treatable with medication
Note: An initial response to PPIs with increasing resistance indicates the success of the operation.
- Patient's desire not to take proton pump inhibitors for life.
- Accompanying hiatal hernia Type II to IV
Note: For hiatal hernias Type II to IV, the hernia itself is already an indication for surgery due to the possibility of severe complications (incarceration).
The operation of the hiatal hernia includes repositioning the herniated content and a hiatoplasty (narrowing of the esophageal hiatus) by suture. Depending on the clinical situation, the procedure is supplemented by sac removal, fundoplication, mesh implantation, or gastropexy.
The laparoscopic or robotically assisted transabdominal approach is nowadays the preferred method for treating hiatal hernia.
The surgical treatment of reflux disease requires a fundoplication in addition to the treatment of the hiatus.
Minimally invasive vs. open
The superiority of laparoscopic fundoplication over open fundoplication is clearly documented in the literature. The guideline explicitly demands that the laparoscopic technique should be used as the standard.
Type of wrap
It has long been controversially discussed whether the partial posterior fundoplication according to Toupet is superior to the total fundoplication according to Nissen in the treatment of GERD. Various studies have attempted to resolve the "Toupet vs. Nissen" controversy.
The full wrap seems to be associated with a higher incidence of postoperative dysphagia and "gas bloating," while persistent reflux symptoms are more common with a partial wrap. In summary, the available data tends to favor the superiority of the 270° Toupet wrap for the treatment of gastroesophageal reflux disease.
Dysphagia
The dysphagia issue has been improved in recent years through the possibilities of endoscopic bougienage. Good results are already seen after 1–2 sessions with large-caliber bougies. In fact, the frequency of reoperations due to persistent dysphagia is rather low.
Sac removal
It is recommended to dissect the hernia sac from the mediastinal structures, which is (not clearly proven) associated with a lower recurrence rate, although it is not always possible with large hernias due to the high risk of iatrogenic injury to the esophagus or gastric vessels.