A hiatal hernia occurs due to a weakening of the diaphragm, where through a gap between the two diaphragmatic crura, varying portions of the stomach, up to the entire stomach in the worst case with spleen and intestinal parts, shift into the thoracic cavity.
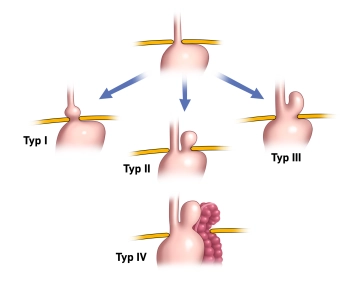
There are 4 types
Type I: Axial hernia, i.e., the stomach entrance shifts along the axis of the organ through the hiatus upward.
Type II: Paraesophageal hernia, i.e., the stomach entrance remains below the diaphragm, and other parts of the stomach shift beside the esophagus through the hiatus into the thoracic cavity.
Type III: Mixed form of Type I and II. There is both an axial shift of the esophagus and stomach towards the thoracic cavity and a displacement of stomach parts up to the entire stomach beside the esophagus (thoracic stomach – "upside-down stomach").
Type IV: The most severe form, where additionally parts of the colon, the spleen with or without the pancreatic tail are displaced into the thoracic cavity.
Axial sliding hernias account for up to 90% of cases and are initially described as a normal variant and not per se as a disease.
The indication for surgery depends on the symptomatology and the morphology of the hernia.
While the goal of antireflux surgery is to strengthen the lower esophageal sphincter with a gastric wrap to prevent reflux, the goal in hiatal hernias of types II-IV is to correct the incorrect position of the stomach and other organs displaced into the thoracic cavity.
An indication for surgery exists for:
- Axial hiatal hernia with therapy-resistant reflux disease
Note: An antireflux operation should only be performed if there is a long-term need for therapy (>1 year).
- Complicated GERD ("gastroesophageal reflux disease"): severe reflux esophagitis (Los Angeles Grade C and D), peptic stricture
The Los Angeles classification is the most commonly used grading system for reflux esophagitis. The Los Angeles classification is based on the endoscopic examination of the esophagus. It distinguishes 4 stages:
- Stage A: One or more mucosal lesions < 0.5 cm. The lesions do not extend beyond the tops of two mucosal folds.
- Stage B: At least one lesion > 0.5 cm. However, the lesions do not yet extend beyond the tops of two mucosal folds.
- Stage C: The lesions exceed the tops of several (>2) mucosal folds. However, they occupy less than 75% of the total circumference of the esophagus, i.e., there are no circular defects yet.
- Stage D: There are circular lesions that occupy more than 75% of the total circumference of the esophagus.
- Disease not completely treatable with medication
Note: An initial response to PPIs with increasing resistance indicates the success of the operation.
- Patient's desire not to take proton pump inhibitors for life.
- Hiatal hernia Type II to IV
Note: For hiatal hernias Type II to IV, the hernia itself is already an indication for surgery due to the possibility of severe complications (incarceration).
The operation of the hiatal hernia includes the repositioning of the herniated content and a hiatoplasty (narrowing of the esophageal hiatus) by suture. Depending on the clinical situation, the procedure is supplemented by hernia sac removal, fundoplication, mesh implantation, or gastropexy.
The laparoscopic or robotically assisted transabdominal approach is nowadays the preferred method for treating hiatal hernia.
The surgical treatment of reflux disease requires a fundoplication in addition to the treatment of the hiatus.
Minimally invasive vs. open
The superiority of laparoscopic fundoplication over open fundoplication is clearly documented in the literature. The guideline explicitly demands that the laparoscopic technique should be used as the standard.
Type of wrap
It has long been controversially discussed whether the partial posterior fundoplication according to Toupet is superior to the total fundoplication according to Nissen in the treatment of GERD. Various studies have attempted to clarify the controversy "Toupet vs. Nissen".
The full wrap seems to be associated with a higher incidence of postoperative dysphagia and "gas bloating", while persistent reflux symptoms are more common with a partial wrap. In summary, the available data tend to favor the superiority of the 270° Toupet wrap for the treatment of gastroesophageal reflux disease. If esophageal function is normal, the 360° full wrap according to Nissen remains a well-documented technique.
Mesh augmentation
The question of whether and in which case a mesh augmentation of the hiatoplasty should be performed is the subject of current discussion. According to the German S2k guideline, reinforcement of the hiatus with foreign material should not be routinely performed. The current data regarding mesh reinforcement of the hiatus does not allow a clear recommendation. On the one hand, advantages of mesh reinforcement regarding the recurrence rate of hiatal hernias have been demonstrated, on the other hand, the risk of a severe complication such as mesh migration into the esophagus with subsequent necessity for resection (e.g., surgery according to Merendino) cannot be neglected.
In current surgical practice, mesh reinforcement is recommended for large hernias to reduce the recurrence rate. However, there are no sufficient long-term data to make a definitive statement for or against the use of a mesh at the hiatus. If a tension-free approximation of the diaphragmatic crura is not possible, mesh reinforcement is definitely recommended.
Also, the type of mesh is ultimately not clarified. Slowly absorbable synthetic and biological meshes seem advantageous, non-absorbable ones should rather be avoided. If a synthetic mesh is to be used, patients must be informed about the risk of mesh erosion.
When fixing the meshes, care must be taken with sharp fixation methods to avoid too deep penetration of adjacent anatomical structures. Injury to the hepatic venous star, the aorta, or the pericardium has been described.
Dysphagia
The dysphagia problem has been improved in recent years by the possibilities of endoscopic bougienage. Good results are already seen after 1–2 procedures with large-caliber bougies. In fact, the frequency of reoperations due to persistent dysphagia is rather low.
Hernia sac removal
Removal of the hernia sac from the mediastinal structures is recommended and is (not clearly proven) associated with a lower recurrence rate, but is not always possible with large hernias due to the high risk of iatrogenic injury to the esophagus or gastric vessels.