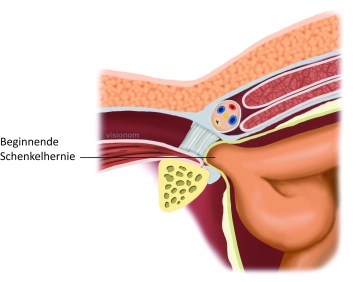
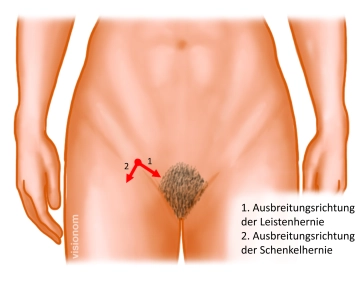
Femoral hernias incarcerate significantly more often than inguinal hernias. Therefore, the indication for surgical treatment should generally be made. However, no diagnostic procedure can distinguish between inguinal and femoral hernias.
Femoral hernia occurs significantly more frequently in women than in men, so every inguinal hernia in women should be operated on promptly.
In the case of femoral hernia, laparoscopic techniques are preferred over open procedures due to less postoperative and chronic pain and the easier placement of the mesh covering all potential hernia orifices. Since ultimately in the described open procedure the mesh is placed in the posterior layer, reoperation is more difficult. The advantage is the lower invasiveness and the possibility to perform the procedure under local anesthesia.
In incarcerated femoral/inguinal hernias, which are distinguished from irreducible hernias by pronounced pain, acute onset, and signs of bowel obstruction, the diagnostic superiority of laparoscopy should be utilized. Its advantage is the possibility of repositioning the incarceration with subsequent assessment of organ perfusion. In about 90% of cases, organ perfusion recovers after repositioning.
The treatment of femoral hernia can be performed immediately or at a later time depending on the local infection situation. In principle, a suture closure of the femoral area is possible even if bowel resection is necessary.