Gastrointestinal tract leakage develops after anastomotic surgical procedures as well as following endoscopic interventions, such as dilation or ablation of precancerous lesions and early cancer, involving endoscopic mucosal resection or submucosal dissection. The risk of postoperative leakage is on the rise because of the increased use of neoadjuvant treatment regimens in esophageal, gastric and rectal cancers.
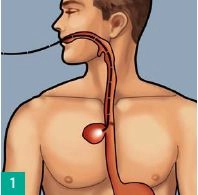
In esophageal resection and extended transhiatal gastrectomy, reconstruction requires an esophageal anastomosis. The failure rate reported in the literature for esophageal anastomoses ranges from 0% to 30%, with mortality rates of up to 50%. The leading cause of mortality in both staple line failure and perforation is developing mediastinitis with severe clinical sepsis.