Since spontaneous healing of rectovaginal fistulas is rather rare, even after fecal diversion by stoma, and conservative measures hardly ever lead to healing, the only adequate treatment is fistula surgery.
Surprisingly enough, many patients present with long-standing fistulas, and this seems to be due to only minor or non-existent burden of suffering and, of course, shame. It is not unusual that the patients present for fistula repair at the urging of their partners or family; sometimes the diagnosis is made incidentally, e.g. in the context of diagnostic work-up and treatment of other disorders.
At the core of the indication for surgical fistula repair are a significant degree of suffering, recurrent infections and any possible continence disorders. If the burden of suffering is not substantial enough and/or if the fistula is asymptomatic, the indication for surgery should only be governed by caution.
When is the ideal time for fistula repair?
Rectovaginal fistulas with a corresponding degree of suffering should be repaired as quickly as possible. However, the condition of the affected tissue plays a decisive role in the timing of the operation.
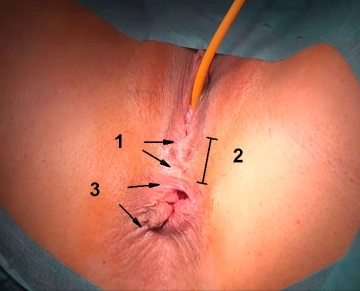
Before initiating surgical treatment, any existing inflammatory processes, e.g. induration and inflammation, must have subsided as much as possible. If a fistula becomes symptomatic during abscess formation, the procedure is initially limited to abscess incision and flagging the fistula with a vessel loop, before undertaking the next step of repairing the fistula. Regular sitz baths, showering, possibly also debridement, a 10-14-day regimen of oral broad-spectrum antibiotics and a diet low in fiber may support the healing of inflammatory reactions.
If the fistula was caused by perineal trauma, e.g. as a complication of the primary repair of a higher-grade perineal tear during vaginal delivery, the patient should wait at least 10-12 weeks after the initial event.
When is a temporary diverting stoma indicated?
Diverting ostomy is indicated in all types of fistulas with marked local inflammatory or scarring changes, extensive tissue defects, as well as anorectal incontinence requiring complex sphincter repair. So-called "complicated fistulas" involve:
- Presence of several fistula openings
- Horseshoe-shaped or suprasphincteric fistulas
- Wide fistula openings, generally requiring difficult closure techniques (e.g. gracilis interposition)
- Marked inflammatory perineal and perianal changes
- Fistulas in Crohn’s disease
- Radiation induced fistula
- Severe obstetric injuries such as loss of perineum
If a diverting stoma is required, the patient should receive detailed advice not only from the surgeon, but also from an ostomy nurse, as well as from self-help groups.
Closure of a diverting stoma should take place no earlier than 3 months after successful fistula repair.
Special case: Rectovaginal fistula in Crohn disease
Fistulas developing in Crohn disease have an extremely poor prognosis with a recurrence rate of over 50%. Regardless of the location of the affected intestinal segment, fistula repair should not be undertaken in acute flare-ups. Surgical measures must be postponed until the episode has subsided, and the indication for a diverting fecal stoma should be broad.